BillingMD360-Aegis guarantees that primary insurance claims will be paid within 2 to 6 weeks of submission. If for some reason any claims are not paid, then BillingMD360-Aegis will reduce the monthly rate for those claims which were not paid within 2 to 6 weeks of submission.
Click here to take a demoWe guarantee this with confidence, as we closely monitor the high hanging fruit, in addition to the low hanging fruit, on your Accounts Receivable.
It is very easy for a billing company to come in and go after easy money that has been left on the table, but it takes knowledge and finesse, to understand a Payer’s Reimbursement Guidelines and apply that to your individual practice.
What makes BillingMD360-Aegis standout, is that we apply all of this knowledge to the RCM process with superior results.
MGMAStat found that only 44.38% of Physicians’ Offices use Certified Coders. 29.96% of Providers do the Coding themselves and not audited.
Many Providers have challenges staying abreast of the ever-changing payer reimbursement guidelines and mandatory requirements. Some of these include:
Best Practices are to have AAPC/AHIMA Certified Coders/Auditors in-house, but it can be costly for a practice to do so.
Under our CES (Continuing Education System) program, our Certified Coders attend Coding/Billing related Events and Conferences and actively participate in AAPC/AHIMA Forums.
It allows our Clients the freedom to go about their daily practice lives and eliminates the need for them to be concerned about any Coding/Billing/Auditing/Compliance Challenges that a payer may present.
The Surveys are in and on average, 15% of Claims are Denied. More than 66% of Providers do not have the proper staff or tools in place to Track and Correct/Appeal Denials.
We have over 20+ years of Medical Coding, Billing & Auditing experience, which has helped us understand the intricacies of Claim Denials that payers often present to the providers who treat their members. This often leads to significant revenue loss, as many back offices, do not have adequate staff with experience who can follow up and appeal denied claims.
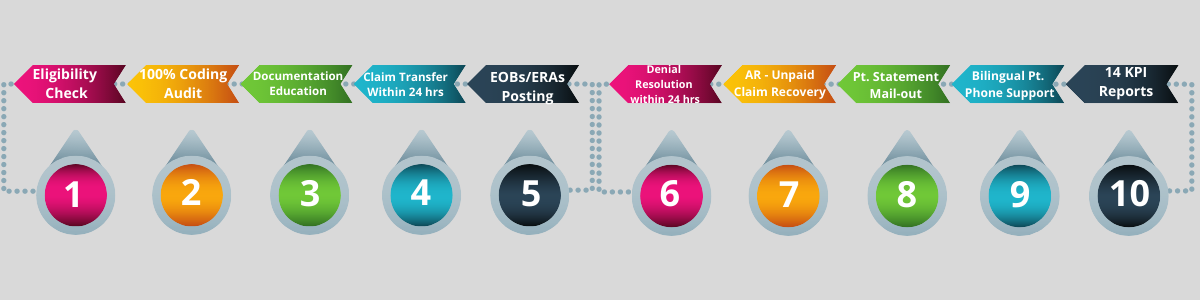
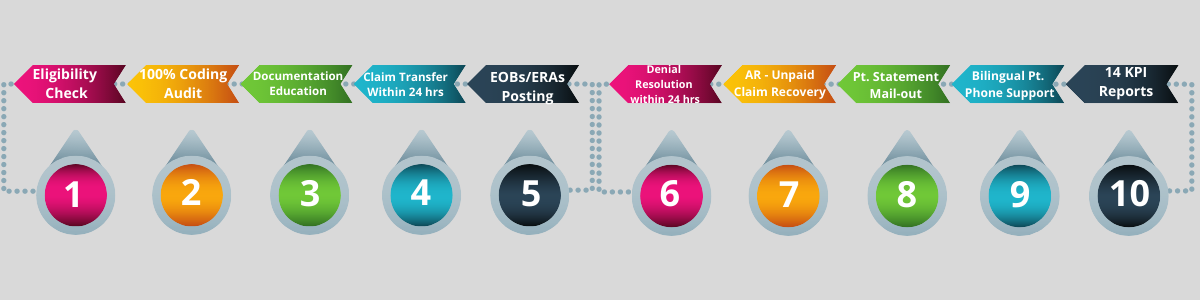
We have developed a tool called AnalyticsStar, which has significantly reduced these ongoing payer reimbursement issues, which does the following: Track, Categorize, Strategize, Correct & Learn (TCSCL).
AnalyticsMD goes beyond the basics and also is able to assist Physicians with tracking 15 different KPIs.
Click here to take a demo








I'm blessed to have a Scribe with Aegis. I'm now able to document the charts per the guidelines and I'm able to sign-off the charts right after seeing my patients.

We are happy with Aegis' Medical Billing and RCM service.

Our AR is under control now. We appreciate Aegis in scheduling Weekly Billing Progress Call, which never skipped even for a single time.